PointClickCare, having promoted interoperability for a long time in a few areas such as senior care, has expanded to include acute care, and particularly to...
ACOs
“Wellness” has become a new mantra for healthcare organizations. Medicare Advantage programs are vaunting their support for “wellness,”...
Company will use funds to continue rapid growth, expand network of 1,000+ practices, and add new wraparound services Aledade announced it has closed a $123...
Led by Enhanced Healthcare Partners, the financing round signals an enormous opportunity for Vytalize Health to accelerate the adoption of value-based care...
Combined company will create one of the largest networks of at-risk providers, improving patient outcomes while lowering costs across the care continuum...
The following is a guest article by Phyllis Wojtusik, RN, Executive VP, Health System Solutions at Real Time Medical Systems. The Centers for Medicare &...
Today, Aledade announced it has closed a $100 million Series D funding round following a year of significant growth for its national network of risk-taking...
Small Wonder Providers Don’t Like Sharing Patient Data For Free. It’s Becoming Their Whole Business.
During the decade or so in which I’ve been following data interoperability, the cleverest people in the healthcare and technology industries have come together...
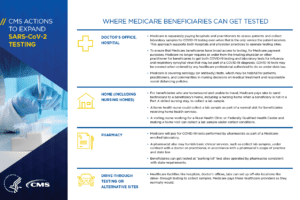
CMS continues to put out massive changes to regulations as they try their best to support healthcare during COVID-19. Yesterday, CMS came out with a bunch...
The following is a guest article by Adam Sabloff, CEO and Founder, VirtualHealth. Health plans, accountable care organizations (ACOs), medical homes, and other...