I’m told that there are only 92 days left for Congress to delay ICD-10 until the deadline to implement ICD-10. A few weeks ago we published a great post from Vishal Gandhi, CEO of ClinicSpectrum, that talked about a part of ICD-10 preparation that is often forgotten: Claims Monitoring.
I know this is going to be a major problem for many healthcare organizations and is going to cause some major cash flow problems if they don’t get on top of their ICD-10 claims by implementing some sort of ICD-10 claims monitoring process. ICD-10 hiccups are the perfect excuse for a payer not to pay your claims.
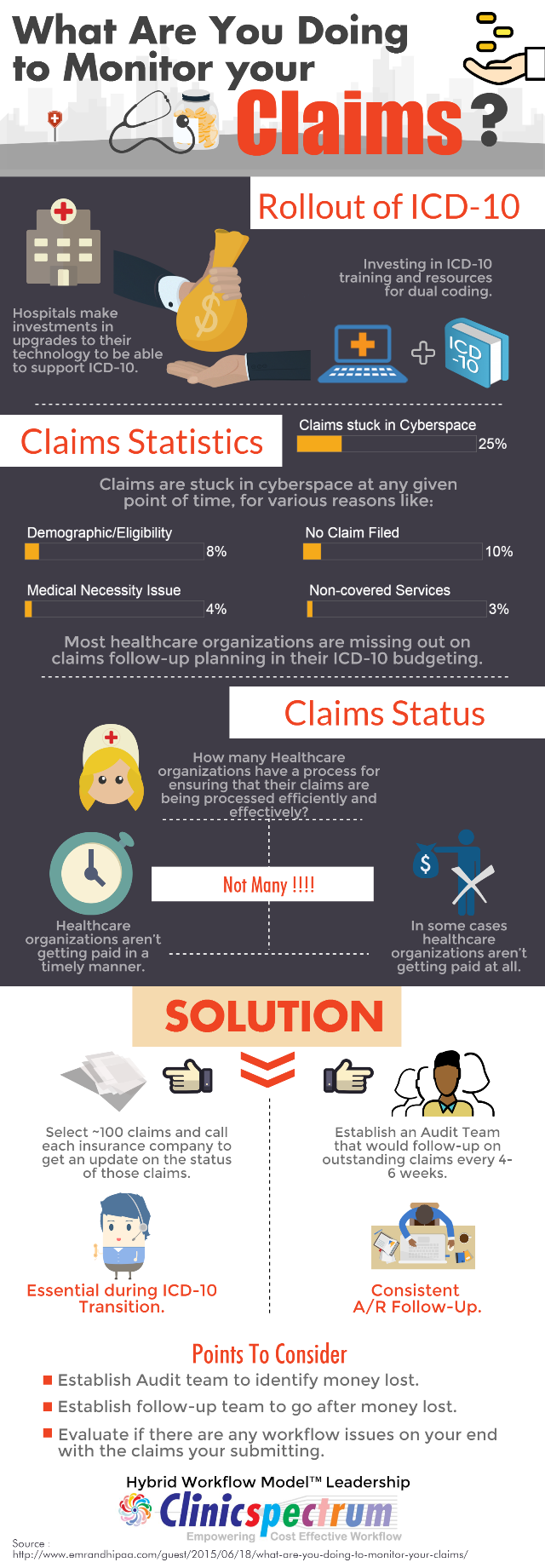
For those that prefer a more visual approach to this discussion, Vishal and his team have put together an infographic that shares the same message as his post. Pretty cool. What won’t be cool is if you’re stuck with a lot of unpaid claims thanks to ICD-10. Make sure you and your organization are ready to deal with it.
Full Disclosure: ClinicSpectrum is a sponsor of EMR and HIPAA.














Even scarier is knowing that a lot of providers still don’t properly monitor or otherwise handle claims under ICD-9. A certain unnamed major lab that we use loses the insurance info, mixes it up with those of other patients OR uses the info from years ago, doesn’t pass through the ICD code received from the physician to the insurance company and far more. Same things happen with a major hospital group by us. Plus every time you get a new bill from EITHER you find you have a new patient number; they look at each visit or test situation as completely new and unique. It’s not unusual to see year old (or worse) bills. And we’re talking routine situations. Imagine where a doctor orders a vaccine to be administered to a patient at a local hospital (unusual, expensive vaccine) but the hospital is incapable of ensuring that (in this case) Medicare knows why something normally not routinely covered should be. An appeal ends up being needed, but there is no one capable of doing it. Patient is on the hook and hospital does not get paid (even what the shot is worth, as opposed to the 20 to 100 times as much that they billed).
However, providers that do it right on 9 and properly take on 10 should, fairly quickly, be in decent shape once 10 comes into play. They will have issues, for instance, with payers that may not yet take 10 (workman’s comp in some states comes to mind). But the ones who always do it right will, I think, continue to do so for the most part, while those who couldn’t handle 9, probably won’t do well on 10.
R Troy,
You’re right about this being a problem for many healthcare organizations under ICD-9 as well. Many healthcare organizations could benefit from claims monitoring today.
I also agree that if a healthcare organization doesn’t have their processes right for ICD-9 will probably have issues under ICD-10 and vice versa. However, I think all healthcare organizations are going to run into payers who aren’t prepared to handle ICD-10 or that have hiccups in their ICD-10 claims processing. I think every healthcare organization is going to need a way to identify which payers are having hiccups with this process and which ones are doing it effectively so they can stay on top of those payers who aren’t paying ICD-10 claims efficiently.
John, good points. One insurer which badly botched the beginning of ACA, is still processing 2014 claims as much as a year old. There is almost an expected failure when you think of them handling current 10 and ancient 9 claims at the same time. And even insurers not this messed up will still have trouble at first even if they do ‘soup to nuts’ claims testing on 10. But ones who are proactive in multi scenario testing ought to do better.
And yes, providers owe it to themselves to monitor payment compliance – at least if they want to stay in business. It would help if practice management tools / software have decent reporting tools; I’m assuming some do, some don’t. But I’m also guessing that many practices wouldn’t bother to use these tools proactively.
Ron